Modern Medicine Relies on Red Blood Cells
Red blood cells (RBCs) are the most common type of cell found in the blood1 and are primarily responsible for delivering oxygen throughout the body.2 Over the years, processing and storage methods have dramatically improved the availability of RBCs for transfusion as a life-saving therapy.
Healthy RBCs contain a number of important elements including ATP and 2,3 DPG, which are critical to transporting and offloading oxygen to the tissues.3,4
RBC Storage is Affected by Donor Variability and Processing
Oxygen levels in RBCs vary between blood donors.5 As soon as blood is collected, RBCs begin to degrade as a result of oxidative damage. Such degradation combined with storage in an oxygen permeable bag reduces the quality, viability, and functionality of RBCs, thereby affecting their ability to deliver oxygen in a patient following transfusion.6,7,8,9 This variability is exacerbated by differing storage times for each RBC unit prior to transfusion.10
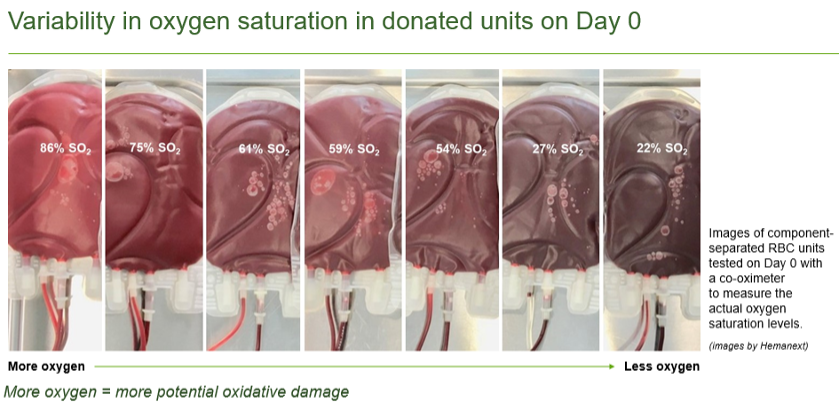
The images in the figure above are from Bardyn et al., and are component-separated RBC units tested on Day 0 that were tested with a co-oximeter to measure their actual oxygen saturation (%SO2) levels. This is an example of RBC unit color as function of oxygen saturation level. It is the Hb that gives their red color to the RBCs, the tint of which depends on how many oxygen molecules are bound by the heme group. RBCs with higher oxygen levels appear scarlet (images on the left) and the images with lower oxygen levels appear darker in color. (images on the right).11
What’s going on in the bag during storage?
See a depiction of the degradation process that occurs during RBC storage and how it impacts the major functions of RBCs in the 3D animation below.
